Managing Care Quality At Scale is Hard
Providers and payers want to deliver excellent care. But without continuous oversight, quality improvements remain out of sight, until it's too late.


Millions of Calls Unchecked
Only 1-5% of clinical interactions and operational processes are audited for training and quality purposes, leaving potential issues undetected

Communication Failures
Clinical communication breakdowns create legal liabilities and reputational risk that threaten organizational credibility and patient safety


Untapped Revenue Potential
CMS awards over $12.7 billion annually in Star Rating bonus payments, representing substantial untapped revenue potential for quality improvements

Complete visibility into care Quality and Risk
Monitor every interaction, identify care gaps, predict risks, and track performance

Monitor
Track interactions, charts, documents, workflows and claims processes

Measure
Generate HEDIS scores, Medication Adherence rates, eCQMs, TEAM and other quality KPIs

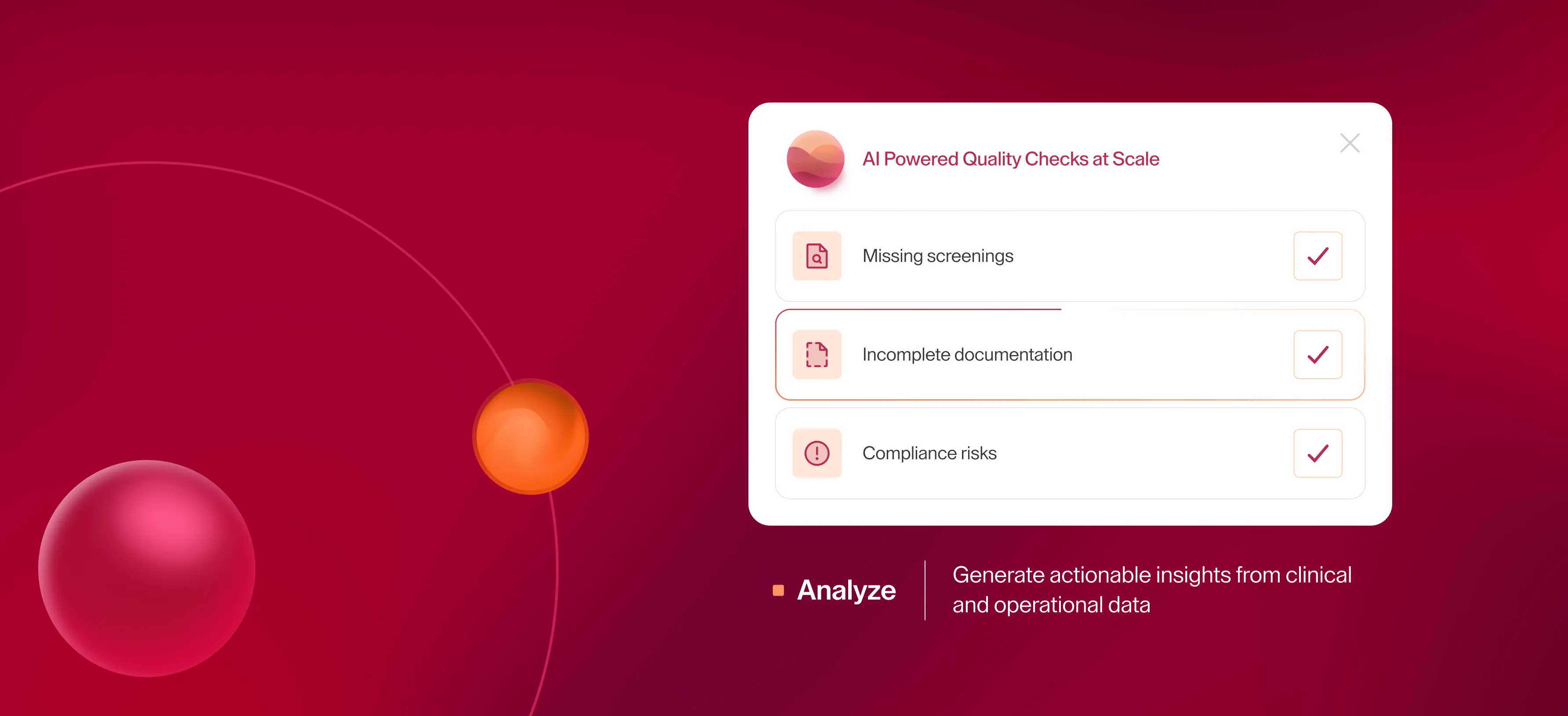
Analyze
Produce interactive dashboards with actionable insights from call and EHR data to identify and anticipate care gaps

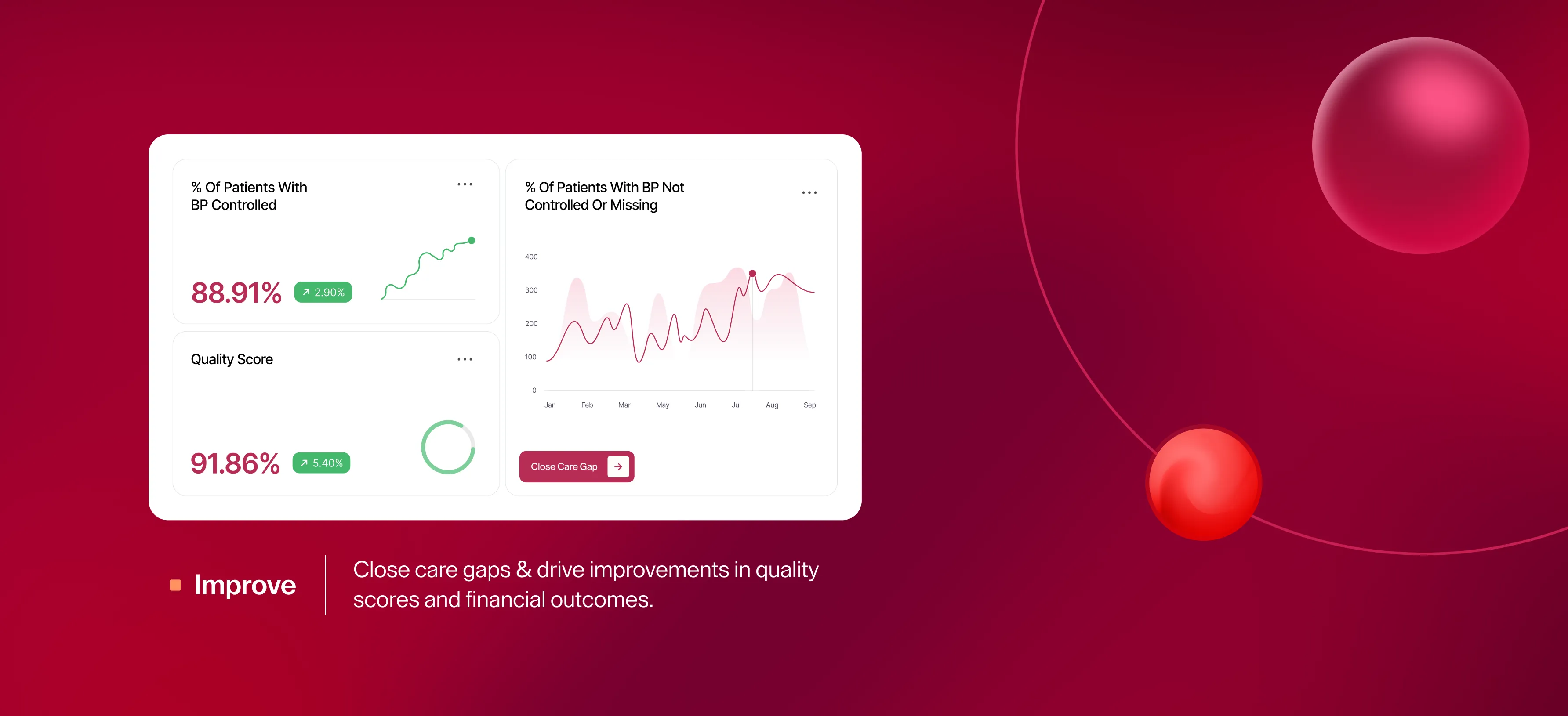
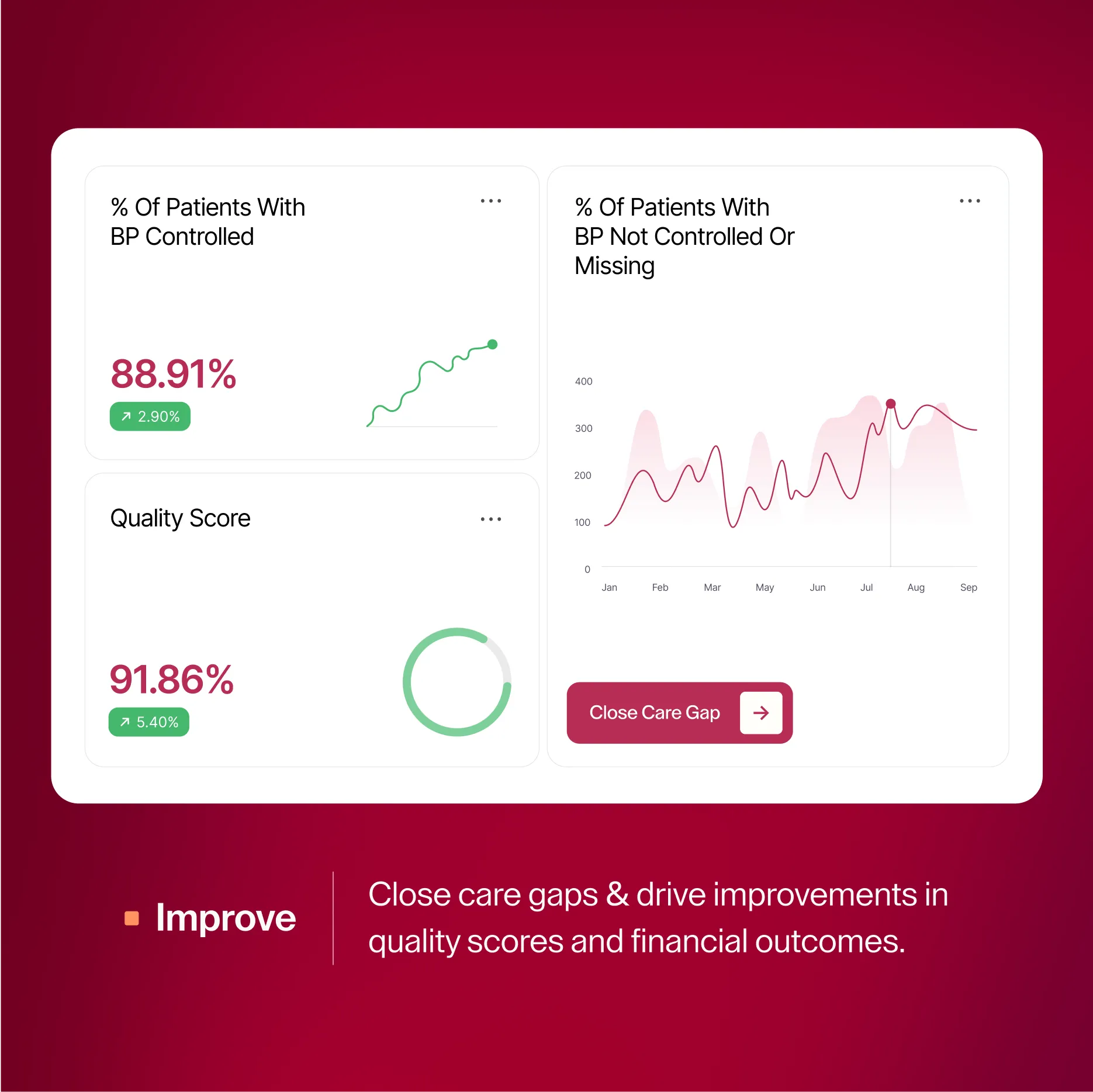
Improve
Achieve proactive care gap closure, and deliver targeted training to improve quality scores & financial outcomes
The problems we solve for our customers
Quality and Risk Management
Ensure call quality and completeness by auditing 100% of calls, rather than sampling just 5%.

Call Audit
Calls are evaluated in multiple languages to screen for appropriate patient evaluation and empathy, resulting in improved care quality, higher patient satisfaction scores, and reduced institutional risk.
Pharmacy Audit
Audit of order entry, dispensing, label accuracy, order pattens etc. to flag anomalies, incomplete documentation, and policy deviations ensuring consistent experience & quality scores across locations
Clinical Guidelines Adherence Monitoring
AI evaluation of clinical practice against local or national guidelines, enabling targeted workforce training for quality improvement.
Star Ratings and Performance Improvement
Automatically identify care gaps, monitor guideline adherence, and track provider performance on value-based care measures.

HEDIS
Continuous oversight of performance for effectiveness of care measures, enabling timely, automated interventions to improve overall scores and payments.
CMS Star Rating
The platform supports quality leaders in improving the proportion of days patients are covered with medications, leading to improved CMS Star ratings and bonus payments.
TEAM
Track and improve performance in TEAM measures for patients having surgery, reduce avoidable hospital readmissions and emergency department use.
Revenue Cycle Optimization
Maximize value-based reimbursements, validate coding accuracy, and identify undercoding opportunities.

Prior Authorization Audit
Our AI audits claims workflows to ensure claims are appropriately coded and processed, accelerating payer reimbursement.
Medical Coding Accuracy
Our AI platform ensures coding accuracy, and revenue integrity while eliminating undercoding opportunities and reducing denial rates through intelligent documentation analysis.
Billing & Claims Audit
Our multi-agent system ensures claims are appropriately coded and processed, accelerating reimbursement from payers.
Proven results across healthcare

Telehealth Communication Quality Improvement
A Nationwide Telehealth Provider
Manual auditing of provider-patient telehealth calls was catching only a small fraction of quality issues, leaving gaps in care delivery and potential risks undetected.
Deployed our multi-agent AI system to evaluate 100% of telehealth consultations for clinical completeness, empathy, and adherence to communication protocols.
Billing & Claims Audit
Healthcare Revenue Cycle Management Company
Manual claims processing created accuracy issues affecting speed of reimbursement.
Our AI audited claims workflows to ensure claims were appropriately coded and processed, accelerating payer reimbursement.

Prior-Authorization Audit
A Florida based Health System
Prior-authorization documents were audited manually to address an increase in denial rates, leading to heavy administrative burden.
Our AI engine audited eligibility and benefits verification, and reviewed clinical documentation for completeness and procedure necessity.



Building better healthcare outcomes through lived experience
We experienced firsthand how healthcare quality gaps, from missed screenings to documentation errors, impact patient care. We saw that health systems need comprehensive tools to monitor and improve quality at scale.
So we built one.
Drawing on our expertise from healthcare delivery, enterprise software, and AI, we created a platform that monitors every clinical interaction to identify care gaps before they impact patient outcomes.
Your data, your control
Privacy and security
SOC 2 Type II, GDPR, and HIPAA certified with end-to-end encryption
Flexible deployment
Self-hosted in your VPC or private cloud, your data never leaves secure environment
Audit-ready
Complete evidence trails with tamper-proof logs for regulatory reviews
Role-based access
Granular permissions aligned with your organizational requirements
Integration Ready
Integration with health records, CRMs, cloud telephony, and cloud providers.